Author: Dr Nicola Cogan
How a Digital Intervention (Sentinel) is Transforming Mental Health Support for Frontline Workers
In recent years, there’s been a growing recognition that psychological trauma is much more than an individual issue - it’s a public health crisis (Cogan, 2024). Frontline workers, including paramedics, firefighters, and police officers, as well as health and social care staff, are particularly affected. These professionals keep society safe and functioning but often face high-stakes situations where trauma is a daily risk. For them, the impact of this trauma can be profound, seeping into every area of life. Yet, finding ways to support their mental health has often been an uphill struggle (Cogan et al., 2024).
As someone who has long worked in mental health care and researched the impacts of trauma on frontline workers, I see this as a particularly crucial time. During the COVID-19 pandemic, I witnessed first-hand the deep-seated impact of trauma on those working in health and social care. Untreated trauma has consequences that reach far beyond the individual, impacting teams, professions, and even communities. And when it’s ignored, the effects are all too familiar: burnout, moral injury, and PTSD. Addressing these risks requires an approach that recognises the intensity and uniqueness of these various roles. This is where Sentinel, a digital mental health platform tailored specifically for frontline workers, comes in.
Currently in its pilot stages, Sentinel is being tested with NHS boards and frontline organisations across the UK. What makes this digital intervention particularly meaningful is that its content was co-created with first responders and health and social care workers. Their insights, feedback, and lived experiences have shaped the tools and resources Sentinel offers. Developed in partnership with mental health professionals, AI specialists, and frontline workers, Sentinel is designed to make mental health care accessible, effective, and private. It understands the individual, the sector, and the job that they do, and that’s part of what makes it so effective. Unlike conventional mental health services, which often operate on rigid schedules, Sentinel offers 24/7 access, allowing frontline workers to get support on their terms. For instance, for a paramedic dealing with a traumatic event in the early hours or a healthcare worker processing a challenging day in the ICU, Sentinel is there. It's always there when they need it most.
Sentinel is designed to be there for people wherever they are, providing accessible, meaningful support that meets both their practical and emotional needs. Stigma around mental health remains a major barrier for many in these professions. Worries about how mental health struggles will be perceived by colleagues or superiors often prevent people from reaching out. Sentinel addresses this issue head-on by creating a confidential, stigma-free, nonjudgmental space. Here, users can engage with mental health resources, whether it’s techniques to manage hypervigilance after a particularly tough call or grounding exercises for when feeling overwhelmed. They can explore these resources in private, breaking down the barriers that keep so many silent.
But Sentinel doesn’t just respond to immediate needs; it looks ahead. Preventive care is at the heart of its design. By offering regular check-ins and tracking changes in mental health over time, the platform empowers frontline workers to recognise signs of stress and anxiety early on. In professions where sustained exposure to trauma can build up without warning, this kind of preventive support is invaluable. One of the things that my research emphasised during the pandemic was the importance of preventive care for frontline staff, who often endure cumulative trauma (Cogan et al., 2022; 2023). This digital intervention brings that same principle into a space that’s accessible to all.
Perhaps one of the most powerful aspects of Sentinel is the sense of community it fosters. Frontline workers often feel isolated, convinced that no one else understands their experiences. Sentinel offers advice and support for peers, family, and loved ones. It provides a means of social connection through sharing experiences of frontline workers that have been through similar challenges, creating a network of shared understanding and support. This peer connection reminds users that they are not alone, countering one of the most insidious effects of trauma: the feeling of isolation.
As Sentinel progresses through its piloting phase, its potential impact on mental health support for frontline workers is becoming clearer. More and more professionals are finding that this new platform (https://sentinel-health.com) could help them manage the intense demands of their roles. It’s a tool that’s not just about coping in the moment but about building resilience and post-traumatic growth for the future. Sentinel is far more than just a digital resource; it’s a new way forward for mental health care in high-stakes professions, proving that accessible, tailored, and stigma-free support can be a lifeline.
With the growing awareness around the mental health needs of our frontline workers, solutions like Sentinel represent a much-needed shift. With support that’s proactive, private, and personalised, Sentinel isn’t just addressing mental health symptoms; it’s helping to build a stronger, more resilient workforce. By doing so, it’s setting a new standard for mental health care in professions that hold the safety and wellbeing of society in their hands.
Note: The Sentinel project is being co-lead by Dr Nicola Cogan & Dr Alison Kirk, Department of Psychological Sciences and Health
References:
Cogan, N. (2024). Psychotraumatology and artificial intelligence: a public health approach. Public Health Open Access, 8(1).
Cogan, N., Archbold, H., Deakin, K., Griffith, B., Sáez Berruga, I., Smith, S., ... & Flowers, P. (2022). What have we learned about what works in sustaining mental health care and support services during a pandemic? Transferable insights from the COVID-19 response within the NHS Scottish context. International Journal of Mental Health, 51(2), 164-188.
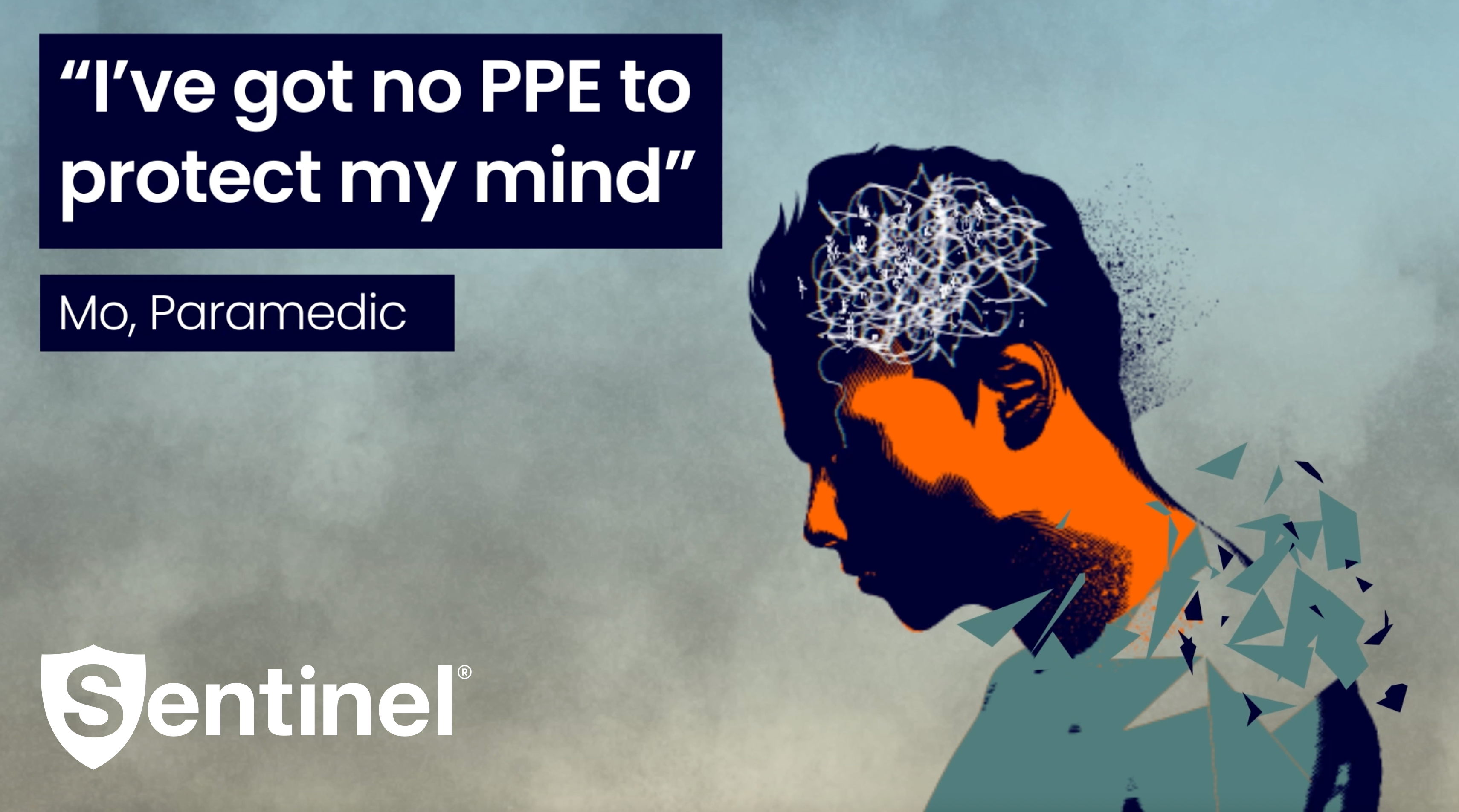
Cogan, N., Craig, A., Milligan, L., McCluskey, R., Burns, T., Ptak, W., ... & De Kock, J. (2024). ‘I’ve got no PPE to protect my mind’: understanding the needs and experiences of first responders exposed to trauma in the workplace. European Journal of Psychotraumatology, 15(1), 2395113.
Cogan, N., Kennedy, C., Beck, Z., McInnes, L., MacIntyre, G., Morton, L., ... & Kolacz, J. (2022). ENACT study: What has helped health and social care workers maintain their mental well‐being during the COVID‐19 pandemic?. Health & Social Care in the Community, 30(6), e6656-e6673.