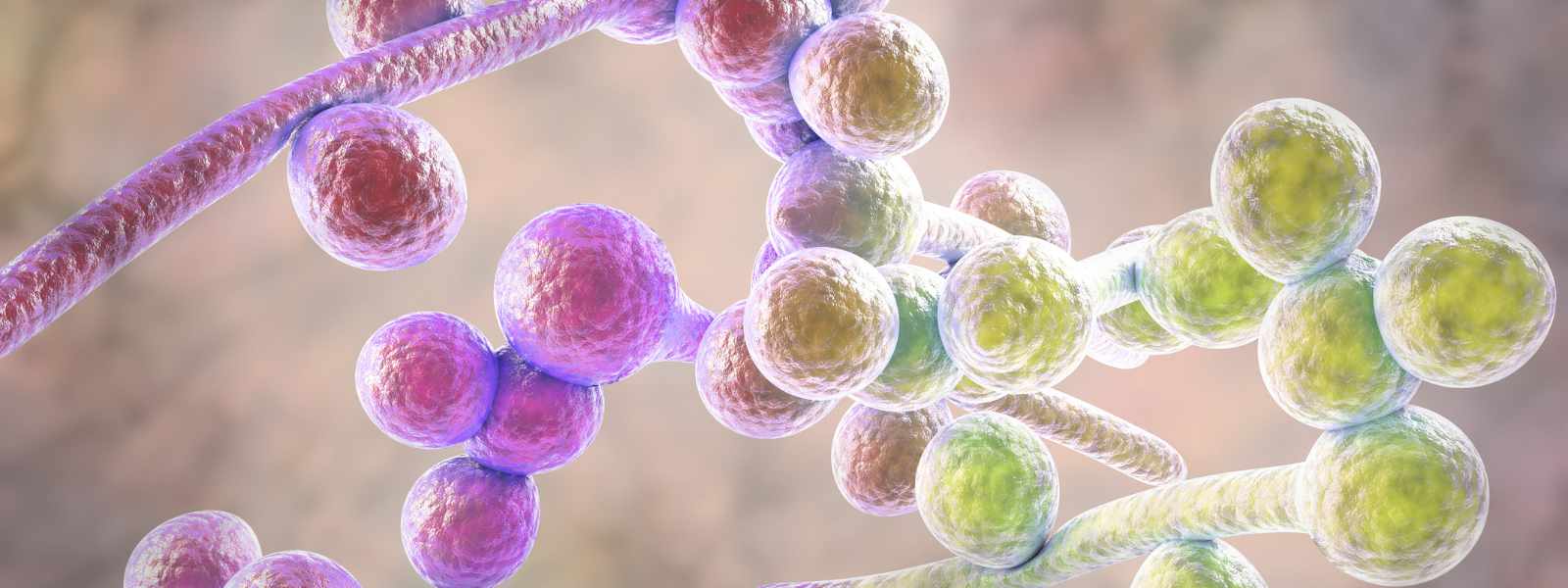
Scientists have shed new light on the yeast Candida albicans, the most common cause of fungal infections worldwide.
Two studies by researchers at the University of Strathclyde in Glasgow reveal how the fungal pathogen is structured at a cellular level and how it forms tough layers called biofilms on medical devices.
Biofilms are a major source of hospital-acquired infections, and cost the NHS more than £2 billion in real terms.
Ultra-detailed views
In the first study the researchers used advanced imaging technology, called stimulated emission depletion microscopy, to reveal ultra-detailed views of the Candida albicans species of the fungus.
They found that dyes normally used for this advanced imaging method do not work well for imaging C. albicans but that a common, low-cost stain is effective for studying live cell structure in more detail than a normal microscope can capture.
This allows for precise tracking of changes in cellular activity over multiple hours. The improved method can help scientists better understand how C. albicans causes disease and develop targeted antifungal treatments.
The findings of the study, a collaboration with scientific equipment supplier Photon Lines as part of a UKRI Engineering and Physical Sciences Research Council (EPSRC) Impact Acceleration Account, are published in the Royal Society journal Open Biology.
Medical devices
The second project looked at how C. albicans and the bacterium Staphylococcus aureus co-infect and stick together to form biofilms on medical devices like catheter tubes or implants. Such biofilms make infections harder to treat and estimates suggest that around 80% of all bacterial infections in humans are linked to the presence of biofilms.
The team created a model using silicone – the same material used in many medical devices – to study how these germs grow and behave together. They found that the shape of C. albicans cells affects how the biofilm forms.
The research aids understanding of how these biofilms take hold on medical devices – a major contributor to infections such as bloodstream infections, pneumonia and urinary tract infections in healthcare settings – and how to stop them. The findings are published in The Journal of Medical Microbiology.
Professor Gail McConnell, Director of the Centre for Biophotonics and the Mesolab at the Strathclyde Institute of Pharmacy and Biomedical Sciences, said: “Our research sheds new light how Candida albicans and Staphylococcus aureus work together to form biofilms on medical devices, making infections harder to treat. By developing a model that mimics real-world conditions, we’re taking a crucial step toward understanding and combating device-related infections that contribute to antimicrobial resistance.
Similarly, by demonstrating the utility of STED microscopy in advancing our understanding of C. albicans biology at the nanoscale, we are providing a platform for future investigations into how fungi cause diseases and how to stop them.
In addition to the EPSRC Impact Acceleration Account funding, the team in the first study was funded by the Leverhulme Trust, and the Biotechnology and Biological Sciences Research Council.
The team in the second study was funded by a Tenovus Small Grant, the Medical Research Council, the Biotechnology and Biological Sciences Research Council, the Leverhulme Trust, the Microbiology Society, the Royal Academy of Engineering Research Chair scheme, and a Medical Research Scotland Daphne Jackson Fellowship.